Coxarthrosis is a disease that affects a patient's hip joints. Treatment is long term. Just a few decades ago, such a diagnosis was practically one sentence for a patient, who promised him: severe fatigue pains, diminished mobility, early disability.
But thanks to the most effective modern treatments, it can not only stop the degeneration process, but also completely cure the disease coxarthrosis in its early stages.
Understanding the cause of the disease has led to the use of an integrated approach to therapy. Treatment for osteoarthritis may include both medications and physical therapy.
What is hip arthritis
Arthritis is a disease in which the normal structure of the cartilage tissue of a joint is broken down. Unlike arthritis, the cause of the deformity is not an infection of the tissues, but a violation of metabolic processes.
Disfigurement of the hip joints, with rare exceptions, is observed in patients over 40 years of age. The development of the pathology is as follows:
- A disturbed metabolism. Cartilage without blood vessels should be nourished by nearby muscle tissue. For various reasons, the synthesis of substances is interrupted.
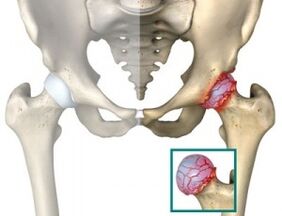
- Due to insufficient nutrition, cartilage begins to lose its elasticity. Over time, it becomes thinner. Heart rate significantly decreased. Grade 3 hip degeneration is characterized by the fact that growths on bone tissue rub against each other. There is practically no cartilage.
- Loads to bones, reduces cartilage thickness, contributes to bone tissue deformation.

After the onset of degenerative changes, it may take many years until the patient develops the third stage of the disease, but in unfavorable cases and non-compliance with preventive measures, thesePathological changes can occur much more quickly.
How the joint disease manifests itself
Symptoms of dry hip disease and their nature depend on the severity of the disease. The most common symptom is pain. Because of the pain that patients often seek professional help. Furthermore, the dullness of the disease is that in the early stages of degenerative changes, as a rule, does not cause major inconvenience, is of a short term nature and is often attributed to common fatigue.
Delays lead to missing out on the best opportunity to start treatment, and curing a second degree of hip disease requires more time and effort. The chance of a successful prognosis remains, as long as therapy is correctly indicated.
The symptoms of the disease are:
- Pain - can occur in the thighs, groin, and in the joint itself. Be wary if pain symptoms appear at rest. This indicates the need to see an urgent joint specialist.
- Difficulty moves, limping. It is observed after prolonged leg immobility, for example, after sleep.
- Over time, the diseased leg is shorter than the healthy leg, the muscle tissue is atrophy, palpable.
In a diagnosis, one cannot do anything without modern diagnostic studies. Therefore, grade 1 hip arthritis is diagnosed only with the help of X-rays, CT and MRI. The picture clearly shows the changes and narrowing of the lumen.
Stages of hip disease
After diagnosis, patient is assigned an ICD 10. This is an international classification of diseases, revised every 10 years.
Thanks to the assigned code, not just the stats are collected. The therapies with the clearest results can be selected. Thanks to international cooperation, over the past time, the treatment of hip joint disease has been significantly improved.
In the real world, it is admitted that degenerative hip disease has three stages or stages of development. Each of them has its own symptoms. Specifically:
- First stage.Painful sensations arise only from overexertion: run, exercise, exercise, etc. v. The pain concentrates mainly in the joint area. Pain usually goes away on its own after a period of rest. In this case, the mobility of the leg remains complete, the muscle strength is not limited. First degree joint disease can only be diagnosed with X-rays or tomography. The picture clearly shows small deformations of bone tissue, not beyond the so-called synovial lips. Joint fissures are slightly narrowed, often in uneven areas.
- Second stage.Characterized by migratory pain that begins to spread down the groin and thighs. Can occur spontaneously at rest. Arthralgia in stage 2 does not go away on its own and the patient must use anesthetic. Range of motion is impaired and muscle tissue atrophy can be observed. The picture clearly shows the growth of bone and deformation of the femur tip. Perhaps the appearance of a cyst in the most heavily loaded part of the thigh - the glial nerve. Diagnosis of joints in the second stage is done quickly. Even on a brief examination, the pathological changes are obvious. An X-ray or MRI is done to see the extent of the malformation.
- Third stage.Chronic onset of pain. Joints can be identified even without thorough examination. The patient cannot move without a cane, there is pelvic tilt leading to short legs. When moving, the patient must tilt the body onto the affected joint. As a result, this leads to even greater degenerative changes. Pictures show enlarged bone deformations. Joint cleft is almost invisible.
Treatment for hip deformity is only effective in the 1-2 stage of the disease. The third stage in the development of the pathology often leads to the need for surgical intervention.
How to treat degenerative hip joints
No matter what medicine you take, hip gymnastics or medication, all methods are based on six basic principles. Specifically:
- Get rid of the pain.
- Provides normal nutrition to cartilage tissue and, if possible, restores it.
- Improves blood flow to the affected area.
- Relieves joint stress.
- Strengthens atrophy muscles.
- Restores joint mobility.
To achieve all six goals, complex therapy is required. So, for example, by prescribing drugs injected into the joint, but without regard to the reduction of the load to the joint, it is possible to lose the beneficial effect of the drug chondroprotectors. It is not surprising that in the real world, 2 to 10 different approaches are often used concurrently, depending on the patient's condition.
How to treat hip disease

The comprehensive hip joint treatment delivers better results than using just one treatment agent - this is a fact recognized by the world's leading joint specialists. Hence, it is not uncommon for a patient to be assigned the following types of treatments simultaneously:
- NSAIDs- nonsteroidal drugs for reducing inflammatory processes are "classic" in treatment. Medicines for osteoarthritis need to be prescribed in combination with nonsteroidal medications or have them in their composition. NSAIDs are particularly effective during an exacerbation of the disease. They help relieve pain and reduce swelling. The reception allows you to perform therapeutic exercises for dry hip, massage, gymnastics and other physical therapy procedures. The downside of NSAIDs is the negative effect on the stomach lining. Patients need to understand that nonsteroidal drugs for osteoarthritis do not cure the disease, but only help eliminate the symptoms, making the treatment possible.
- Chondroprotectors and hyaluronic acid.These drugs are a new phase in the treatment of the hip joints, so they can be grouped together.
- Chondroprotectors are prescribed as restorative therapy. With prolonged use, the chondroprotectors restore damaged cartilage tissues, but their effectiveness is limited by the early stages of the disease.
- Hyaluronic acid forms a layer between bones, helping joints relieve stress. Effective as a restorative therapy.
- Muscle relaxants- are vasodilators and may reduce muscle spasm. It is prescribed to reduce the load to the joint. Muscle relaxants can be used only as part of complex drug therapy.
- Ointment- although advertised for ointments as a miracle cure for disease, in fact they only eliminate the unpleasant symptoms of the disease. On the other hand, analgesics in the form of an ointment enhance the effectiveness of conservative treatment, allowing you to reduce puffiness and alleviate the patient's condition.
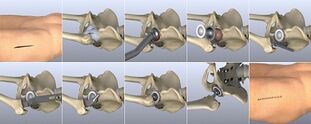
- Intra-joint injection- designed to relieve pain, restore cartilage or protect from excessive pressure on the joint. The most commonly used drug is corticosteroid. They relieve pain by allowing patients to initiate physical therapy. The corticosteroid group may also include hyaluronic acid preparations. The effectiveness of injecting drugs in the joint largely depends on the experience of the surgeon (statistically, 30% of doctors performing the operation have missed the joint).
Some drugs can be harmful to the body. It is strictly forbidden to self-medicate!
The hip bandage will reduce the stress on the joints and reduce factors, the main cause of tissue irritation that leads to the inflammatory process. Therefore, in conjunction with drug therapy, immobilization of the affected area is often prescribed.
Alternative methods and physiotherapy
In addition to prescribing anti-inflammatory drugs, intra-articular injections and other drugs, the patient can undergo physical therapy and use the help of non-traditional therapies.
- Manual therapy- this is more gentler on damaged tissue than massaging the hip joints to treat osteoarthritis. Any strong impact on the affected area can easily provoke the inflammatory process. In our region, manual therapy is not yet popular, but in the West it is widespread and is one of the official therapies.
- Physiotherapyfor the treatment of deformity of the joints is a wide area where patients can choose between traditional and non-traditional methods. With degenerative hip disease, Pilates, yoga is popular, as well as water exercises and other methods to restore the function of atrophied muscles. Moderate physical education and exercise, along with medication, have a beneficial effect and contribute to the recovery of the patient.
- Traditional Medicine- most arthologists oppose this approach as independent therapy. And their opinion is plausible. A large number of patients who refused the help of traditional medicine became self-disabled. But under the supervision of a specialist, effective treatment of degenerative hip disease with folk remedies is completely possible. Most herbs and infusions used have anti-inflammatory and analgesic effects. Some drugs have serious contraindications, you should consult a joint specialist before taking. Unique alternative treatments for hip disease treatment are recommended with caution. Some formulations not only do not contribute to improvement but also lead to the opposite effect, stimulating faster cartilage destruction.
- Homeopathy- helps to normalize the synthesis of substances in the body. Homeopathy is especially effective in post-traumatic joint disease, allowing you to cope with the main factors that lead to the development of the disease.
- Apitherapy- the bee sting treatment is very effective, it allows you to combine the effects of acupuncture and drug therapy. It's no surprise that many effective and warming ointments contain treated bee venom. Apitherapy is usually more effective than hip block. The effectiveness of using apitherapy therapy should be determined by the attending physician.
- Magnetic therapy- is used as an adjunct and preventive treatment. The effect of magnets increases blood flow to tissues, helping to restore metabolic processes. Remove salt residue.
- Hirudotherapy- leech therapy has been in use for several centuries. It has been shown that leech saliva entering the blood contains a substance that promotes its liquefaction. As a result, the blood can even enter the capillaries and atrophy of blood vessels.
- Mud therapy- has a mild warming effect, helping to obtain the necessary nutrients. Correct application of sludge therapy reduces inflammation and pain. It is forbidden with purulent arthritis of the hip joint. It is prescribed with caution in the presence of blood clots and vascular disease.
- Shilajit for arthritis- used both in its pure form and as part of tincture and suppositories. The beneficial substances that make up Mumiyo promote tissue regeneration. Mumiyo is especially effective in the early stages of the disease.
- Self-massage- Get rid of pressure and clap hard. When massaging, it is necessary to ensure the circulation of blood and lymph. A chiropractor or an experienced massage therapist will point out the types of movements and their directions.
Treatment of osteoarthritis at home by folk methods must provide reasonable nutrition.
Losing just 5 kg of weight will reduce the likelihood of initiating an inflammatory process by about 30%.
Arthritis and pregnancy
Pregnancy with degenerative hip joint causes double stress on a woman's body. Most of the drugs are banned during pregnancy. At the very least, they must be taken care of so as not to harm the baby.
If hip arthritis during pregnancy is in its early stages, it is recommended that drug therapy be postponed until after childbirth.
May be born with hemophilia, but it is important to understand all the risks associated with this. Complications after childbirth are not uncommon, and the deformation of cartilage tissue occurs at an increasingly rapid rate.
Even during the planning of a baby, it is necessary to examine the whole body. All medications, ointments, and pain relievers are for use only as directed by a doctor.
Consequences of joint disease
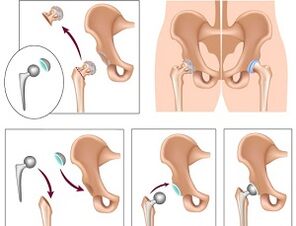
In the late stages of the disease it is not possible to cure coxarthrosis in the usual way. Surgery is needed. This activity is a last resort and can be done in a variety of ways.
- Joint replacement- complete restoration of all motor functions. The downside of this solution is that the life of the prosthesis is limited. On average after 15 years there will be a second implementation to replace it.
- Laser therapy for the surgical hip joint- is used in the case of partial rejection of a bone joint. Using laser therapy, the damaged surface is removed and replaced with an artificial insertion.
All surgeries are temporary, but without them the patient will be disabled.
Early diagnosis of coxarthrosis and a correctly prescribed rehabilitation therapy is the only reliable way to fight the disease. Ignore symptoms that lead to disability.





































